Postpartum Anxiety (PPA) & EPDS: Signs, Symptoms, and PPD Differences
August 4, 2025 | By Clara Maxwell
Becoming a mother is an incredible journey, filled with incredible highs and unexpected challenges. While society often focuses on the joy, many new mothers quietly struggle with overwhelming emotions. You might find yourself constantly worried, unable to relax, or feeling a sense of dread you can’t shake. How do you know if what you're feeling is normal worry or something more, like postpartum anxiety?
This guide is here to offer clarity and support. We will explore the nuances of postpartum anxiety (PPA), helping you identify its signs and understand how it differs from the more widely discussed postpartum depression (PPD). Gaining knowledge is the first step toward taking control of your mental wellness. If you are looking for a starting point to understand your feelings, you can always take a free screening to assess your emotional state.
What is Postpartum Anxiety (PPA)?
Postpartum anxiety is a mood disorder that can affect women during pregnancy and after childbirth. While it's normal for any new parent to worry, PPA is different. It involves intense, persistent anxiety that can interfere with your daily life and your ability to care for yourself and your baby. Unlike the "baby blues," which typically fades within a few weeks, PPA can linger and intensify without proper support.
This condition is more than just feeling stressed. It involves an overwhelming rush of racing thoughts and physical symptoms. Understanding what PPA looks like is crucial for recognizing it in yourself or a loved one and taking the next step toward feeling better.

Common Signs & Symptoms of PPA
The experience of PPA can vary, but certain patterns are common. You might feel a constant sense of unease or find your mind racing with "what if" scenarios, often centered on your baby's health and safety. These thoughts can be intrusive and hard to control.
Here are some of the most reported PPA signs:
- Constant, uncontrollable worry: Anxious thoughts that loop in your mind.
- Feelings of dread: A persistent sense that something terrible is about to happen.
- Irritability and restlessness: Feeling on edge and unable to settle down.
- Physical symptoms: These can include a racing heart, shortness of breath, dizziness, nausea, and muscle tension.
- Sleep disturbances: Difficulty falling or staying asleep, even when the baby is sleeping.
- Changes in appetite: Either eating much more or much less than usual.
Recognizing these symptoms is a vital act of self-awareness and the first step towards getting the support you deserve.
Understanding Anxiety After Birth: Beyond Worry
The anxiety after birth associated with PPA goes far beyond the typical concerns of a new parent. While a new mom might worry if her baby is eating enough, a mom with PPA might lie awake for hours, consumed by irrational fears of harm coming to her child. This level of anxiety is not a reflection of your ability as a parent; it is a symptom of a treatable medical condition.
This form of perinatal anxiety can make it difficult to enjoy motherhood. Instead of bonding, you may feel detached or overwhelmed by the responsibility. It's essential to remember that you are not alone in this experience, and support is available. Taking a moment to check in with yourself through a confidential online test can be an empowering way to understand your feelings.
PPA vs. PPD: Key Differences to Know
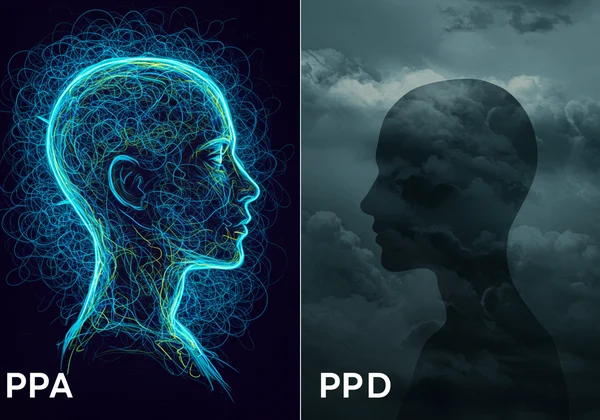
While often discussed together, Postpartum Anxiety (PPA) and Postpartum Depression (PPD) are distinct conditions, though they can co-occur. Understanding the PPA vs PPD distinction is vital for getting the right diagnosis and treatment. The primary difference lies in the core emotional experience. PPA is dominated by fear and worry, while PPD is characterized by persistent sadness and loss of interest.
Many new mothers feel confused about their emotions, wondering if their intense worry is a sign of depression. While both can share symptoms like sleep problems and irritability, their emotional foundations are different. A clear understanding helps you articulate your feelings to a healthcare provider, leading to more effective support.
Emotional Landscapes: Beyond Sadness and Fear
Think of PPA and PPD as different emotional landscapes. PPD often feels like a heavy, gray cloud of sadness, hopelessness, and emptiness. You might struggle to feel joy, even in moments you "should" be happy. The world can seem muted, and you may withdraw from loved ones.
In contrast, the landscape of PPA is one of high alert and agitation. It's characterized by a constant hum of anxiety, punctuated by spikes of panic and obsessive worry. Rather than feeling numb, you might feel overly stimulated and unable to turn your mind off. Recognizing this core difference in your perinatal anxiety is key to finding the right path forward.
Overlap and Co-occurrence: Why Both Can Appear
To make matters more complex, it is very common for PPA and PPD to exist at the same time. Research suggests that about half of women with PPD also experience significant anxiety symptoms (learn more about perinatal mental health from NIMH). The relentless worry of PPA can be exhausting, leading to feelings of hopelessness characteristic of PPD. Conversely, the low energy and motivation of PPD can make it harder to cope with anxiety.
Because of this overlap, a comprehensive screening is important. Tools designed to assess perinatal mood disorders can help identify the full spectrum of your symptoms. For instance, an initial EPDS depression screen can provide valuable insights that you can then discuss with a healthcare professional.
When to Seek Support for Perinatal Mental Health
If your feelings of anxiety or sadness are persistent, overwhelming, and impacting your ability to function, it is time to seek support for your perinatal mental health. You do not have to wait until you reach a crisis point. Acknowledging that you need help is a sign of strength, not weakness. Your well-being is essential for both you and your baby.
The perinatal period is a time of immense change, and it's okay to need support navigating it. Help can come in many forms, from professional therapy and medical advice to simple coping strategies you can implement at home. The most important step is reaching out.
Initial Coping Strategies for Managing Anxiety
While professional help is crucial for treating PPA, there are several initial coping strategies you can use to manage symptoms in the moment. These techniques can help ground you when you feel overwhelmed.
- Mindful Breathing: When you feel your heart racing, focus on taking slow, deep breaths. Inhale for four counts, hold for four, and exhale for six. This can help calm your nervous system.
- Talk About It: Share your feelings with a trusted partner, friend, or family member. Voicing your fears can lessen their power.
- Gentle Movement: A short walk outside can help clear your head and reduce feelings of restlessness.
- Focus on the Senses: When thoughts are racing, ground yourself in the present. Name five things you can see, four things you can feel, three you can hear, two you can smell, and one you can taste.
These strategies are tools, not cures, but they can provide immediate relief and empower you to manage difficult moments.

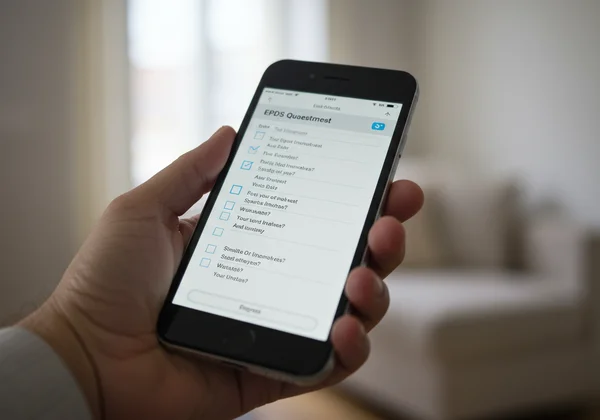
The Role of Screening Tools Like EPDS in Assessment
Screening tools are a vital first step in identifying perinatal mood and anxiety disorders. The Edinburgh Postnatal Depression Scale (EPDS) is a globally recognized questionnaire designed to detect symptoms of PPD. While its name focuses on depression, several of its questions directly address feelings of anxiety, worry, and self-blame, making it a valuable tool for identifying risk for PPA as well.
Taking a confidential and free EPDS screening online provides a quick, private way to assess your symptoms. The results give you a concrete starting point for a conversation with your doctor or a mental health professional. It transforms vague feelings into measurable data, helping you advocate for your own health. You can start your screening now to get a better understanding of your emotional well-being.
Taking Control: Your Next Steps in Perinatal Wellness
As you navigate the emotional challenges of motherhood, remember you don’t have to do it alone. Understanding the signs of postpartum anxiety and how it differs from PPD is a crucial act of self-empowerment. PPA is real, common, and highly treatable. By recognizing the symptoms, exploring coping strategies, and knowing when to seek help, you are taking control of your perinatal wellness.
Remember, your mental health is a priority. Using a confidential screening tool can be an excellent first step to understanding what you’re experiencing. We encourage you to visit our homepage to take the free, science-backed EPDS screening. Share your results with a healthcare provider to create a personalized plan for your well-being.
Frequently Asked Questions About Perinatal Anxiety & Screening
Does EPDS screen for anxiety?
While the Edinburgh Postnatal Depression Scale (EPDS) is primarily designed to screen for depression, it is highly effective at identifying anxiety as well. Several questions on the scale, particularly those asking about feeling anxious or worried for no good reason, can indicate a risk for PPA. A high score often warrants a comprehensive evaluation for both depression and anxiety.
What is a normal EPDS score?
There isn't a single "normal" score, but rather score ranges that suggest different levels of risk. Generally, a score of 0-8 is considered low risk. A score of 9-11 suggests the possibility of mild depression, while a score of 12 or higher indicates a likely risk of a depressive illness and that a professional consultation is highly recommended. To see where you fall, you can get your EPDS score confidentially.
How long does the EPDS test take?
The EPDS test is designed to be quick and straightforward. It consists of 10 questions and typically takes only 3 to 5 minutes to complete. This makes it an accessible first step for busy new parents who want to check in on their mental health without a significant time commitment.
What to do after a high EPDS score?
Receiving a high EPDS score is not a diagnosis, but it is an important signal to seek professional support. The first and most critical step is to schedule an appointment with your healthcare provider, such as your OB/GYN, primary care physician, or a mental health professional. Share your score and your symptoms with them to discuss the best next steps, which may include therapy, medication, or other support services.