Your EPDS Results: From AI Analysis to Personalized Action Plan
December 25, 2025 | By Clara Maxwell
Are you looking at your EPDS results and wondering, "What do these scores mean for me, and what should I do next?" You're not alone. After completing a perinatal depression screening, understanding how to turn those numbers into meaningful action is the most important step. Many new and expectant parents feel a mix of relief and uncertainty after seeing their results.
This guide is here to help. We'll walk you through how to interpret your results, especially the advanced insights from our optional AI-powered report. Using real-life (but anonymized) examples, we will show you exactly how to transform your insights into a personalized care plan that fits your unique situation. If you haven't taken the screening yet, you can get a clear, confidential picture of your emotional well-being with our free online screening.

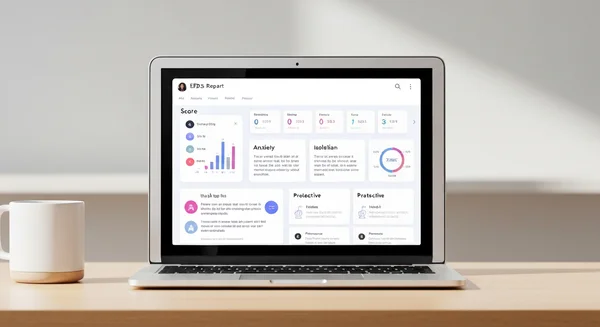
Understanding Your EPDS AI Report: What Each Element Means
Taking an EPDS screening is a proactive step toward understanding your mental health. The basic score gives you a valuable snapshot. Our optional AI-powered report provides a deeper analysis. It goes beyond the numbers to offer personalized context. Let's break down what you'll find in this report.
Decoding Your Score Breakdown
Your total score, ranging from 0 to 30, is the first piece of information you'll see. This score places your self-reported symptoms into a general risk category—low, moderate, or high. However, the AI report breaks this down further. It analyzes which specific questions contributed most to your score, helping you see patterns. For instance, it might highlight that your score is primarily influenced by feelings of anxiety or difficulty sleeping, rather than general sadness. This breakdown helps pinpoint the exact areas that need the most attention.
How the AI Identifies Key Risk Factors and Protective Elements
Our unique AI analysis doesn't just look at symptoms; it also identifies underlying themes. By examining your answers, the AI can highlight potential risk factors, such as a lack of social support or overwhelming feelings of guilt. At the same time, it looks for protective elements—your strengths. It might identify that you still find moments of joy or feel a strong connection to your baby, even while struggling. Understanding both your vulnerabilities and your strengths is crucial for building an effective and balanced action plan.
Making Sense of Personalized Recommendations
Based on its analysis of your unique risk and protective factors, the AI generates personalized recommendations. These aren't generic suggestions. Instead, they are tailored to the themes identified in your perinatal mental health assessment. If anxiety was a major contributor to your score, the report might suggest specific mindfulness techniques. If a lack of support was indicated, it might recommend conversation starters for talking with your partner or family. These recommendations are your first step toward creating a concrete plan.
Case Study 1: Emma's Journey from Score 12 to Personalized Care Plan
To see how this works in practice, let's look at Emma's story. Emma was a mother to a two-month-old. She felt constantly on edge and exhausted. She wondered if this was just 'normal' new-mom stress. That's why she decided to take the online depression screening.
Emma's Initial Screening Results and AI Analysis
Emma received a score of 12, which falls into the moderate-risk range for perinatal depression. The basic result concerned her, but the AI analysis gave her clarity. The report highlighted that her highest-scoring answers were related to anxiety and an inability to laugh and see the funny side of things. It also noted a protective factor: her answer to question 2 indicated she still enjoyed looking forward to things sometimes. This insight was empowering; it showed her she wasn't completely lost in her feelings.
Creating Emma's Targeted Interventions Based on AI Insights
Emma's AI report suggested a few targeted interventions. Since anxiety was a key theme, the report recommended trying a guided breathing exercise for five minutes twice a day. To address her loss of enjoyment, it suggested scheduling one small, pleasurable activity daily, like listening to a favorite podcast during her baby's nap. Finally, it provided a script to help her talk to her partner about feeling overwhelmed.
Measuring Progress: Follow-up Screening and Adjustments
Emma followed the recommendations for two weeks and started feeling a slight but noticeable improvement. She felt more in control and less alone. Following the advice in her report, she shared her results with her doctor, who confirmed she was experiencing postpartum anxiety and recommended a local support group. Emma decided to retake the screening four weeks later. Her score had dropped to 8, showing her that the small, consistent steps she was taking were making a real difference.

Case Study 2: Michael's Experience Using the Scale as a Supportive Partner
Perinatal mental health challenges don't just affect mothers. Partners are often the first to notice something is wrong but may not know how to help. Michael was worried about his wife, Sarah, who had become withdrawn and tearful after their son was born.
Understanding the Partner's Perspective: How Michael Recognized Warning Signs
Michael noticed that Sarah wasn't sleeping even when the baby was, had lost her appetite, and often seemed distant. He remembered reading about postpartum depression and gently suggested they look into it together. He found the screening tool and proposed that Sarah take it, assuring her it was completely confidential and just a way to gather information. This approach made Sarah feel supported rather than judged.
Translating the AI Report into Actionable Support Strategies
Sarah's score was 15, indicating a high probability of depression. The AI report identified significant feelings of guilt and self-blame. For Michael, this was a revelation. He realized Sarah wasn't just tired; she was battling intense internal criticism. The report’s recommendations for partners included validating her feelings ("It makes sense you feel this way; you're going through so much") and taking over specific household duties without being asked. This shifted Michael’s role from a concerned observer to an active supporter.
Communication Strategies for Discussing Results with Your Partner
The AI report provided sample conversation starters for Sarah to use with Michael, but it also helped Michael know what to say. Armed with the report's insights, he was able to start a conversation by saying, "I read through the report, and it seems like you've been putting a lot of blame on yourself. I want you to know I'm here with you, and we're a team." This opened the door for a more honest conversation, strengthening their partnership and encouraging Sarah to seek professional help. If you're concerned about a loved one, suggesting they start a screening can be a gentle and effective first step.
Converting AI Insights into Your Personalized Action Plan
An AI report is full of valuable information, but its true power is unleashed when you use it to create a personalized action plan. This plan doesn't have to be complicated. It's simply a set of manageable steps to support your mental well-being.
Step 1: Prioritizing Recommendations Based on Your Highest Risk Areas
Look at your report and identify the top 1-2 themes the AI flagged as key risk areas. Is it anxiety? Lack of sleep? Social isolation? Start there. Choose one or two of the simplest recommendations related to that theme. For example, if sleep is the biggest issue, your first step might be to commit to a 20-minute nap when your baby naps, instead of trying to overhaul your entire nighttime routine. Small wins build momentum.
Step 2: Integrating Professional Support into Your Action Plan
This screening tool is not a diagnostic one. A crucial part of any action plan is involving a professional. This could be your family doctor, an OB/GYN, a midwife, or a mental health therapist. Your AI report can be an incredibly useful tool in these conversations. Schedule an appointment and bring your results with you. This shows you've done your homework and helps your provider understand your situation quickly.
Step 3: Building Daily Practices Based on Your Analysis
Your action plan should include small, daily habits that align with the insights from your report. If the AI identified a lack of self-care, your daily practice might be a five-minute stretch in the morning. If it highlighted feelings of isolation, it could be a commitment to text one friend each day. These practices are not about fixing everything at once; they are about creating consistent moments of support for yourself throughout the day. To begin building your plan, you first need your results. Take the test online to get started.

Sample Dialogue: Discussing Your Results with Healthcare Providers
Talking to a doctor about your mental health can be intimidating. Many people worry they won't be taken seriously or won't know what to say. Your report is a powerful tool to make this conversation easier and more productive.
What to Say When Your Score Suggests Moderate Risk
If your score is in the moderate range (e.g., 10-12), you can start the conversation clearly and confidently.
- You could say: "I recently took the Edinburgh Postnatal Depression Scale online, and my score was 12. The results suggest I might be at moderate risk for postpartum depression, and I wanted to discuss it with you."
This direct approach immediately gives your doctor context and signals the seriousness of your concern.
Presenting Your AI Analysis to Maximize Consultation Time
Doctor's appointments are often short. Your AI report helps you make the most of every minute. Instead of just saying "I feel bad," you can provide specific details.
- You could say: "My screening report highlighted that anxiety and feelings of being overwhelmed are my biggest issues right now. It also noted that I'm still able to enjoy some things, but I'm worried about the anxiety getting worse. What do you think would be a good next step?"
This helps your doctor quickly pinpoint the problem and move toward solutions.
Questions to Ask Your Doctor Based on Your Report
Your report can also help you formulate questions for your doctor. Being prepared with questions ensures you leave the appointment with the information you need.
- Based on a high score for anxiety, you could ask: "My report showed high levels of anxiety. Are there specific resources or therapies you recommend for postpartum anxiety?"
- Based on a theme of isolation, you could ask: "I've been feeling very isolated, which my report picked up on. Do you know of any local new parent support groups?"
Using your report turns a potentially vague conversation into a focused, collaborative problem-solving session.

The Takeaway
Getting your EPDS score is just the first step. Understanding what it means and taking action is where your real journey to better mental health begins. By understanding how to interpret your AI-powered report, you can transform screening data into a powerful tool for your well-being. Creating a personalized action plan and communicating effectively with healthcare providers are the key steps to turning insight into meaningful support.
Keep in mind that your Edinburgh Postnatal Depression Scale results reflect how you're feeling right now. This snapshot of your mental health can change, and it's not a permanent label. They are an instrument of empowerment, giving you the knowledge and confidence to take control of your mental health. The best thing you can do for yourself now is take one small, manageable step forward.
Ready to take the first step on your personalized care journey? Start with a free, confidential EPDS screening today.
Frequently Asked Questions About Reports and Action Plans
What should I do immediately after receiving my results?
First, take a deep breath. Your results are information, not a judgment. If your score is high or you have any thoughts of harming yourself (related to question 10), please contact a crisis hotline or your local emergency services immediately. Otherwise, take some time to read through the AI analysis. Identify one small, manageable recommendation and consider scheduling an appointment with your healthcare provider to discuss the results.
How often should I retake the screening to monitor my progress?
Many experts recommend retaking the screening every 2 to 4 weeks if you are actively working on an action plan or treatment. This allows you to track your progress and see if your strategies are working. Regular check-ins can be very motivating. You can try our free tool anytime you need to check in with yourself.
Can the AI analysis replace consultation with a healthcare provider?
No, absolutely not. The AI analysis is a powerful educational tool that provides personalized insights and guidance, but it is not a substitute for professional medical advice, diagnosis, or treatment. Always consult with a qualified healthcare provider about any mental health concerns. The report is designed to support, not replace, that crucial relationship.
How accurate is the AI analysis compared to professional interpretation?
The EPDS scale itself is a clinically validated tool used by professionals worldwide. Our AI analysis is designed to mimic the thematic interpretation that a trained professional might perform, by identifying patterns and connections between your answers. It provides a structured, data-driven perspective that can be very helpful, but the nuanced understanding and diagnostic skill of a human expert are irreplaceable. Think of the AI report as an excellent starting point for a deeper conversation with a professional.