การสนับสนุนคู่ของคุณ: คู่มือ EPDS สำหรับ ภาวะซึมเศร้ารอบการคลอด
October 11, 2025 | By Clara Maxwell
เมื่อทารกน้อยถือกำเนิดขึ้น นั่นคือช่วงเวลาแห่งความสุขอย่างท่วมท้น แต่ก็อาจนำมาซึ่งความท้าทายที่ไม่คาดคิด หากคุณสังเกตเห็นว่าคู่ของคุณไม่เป็นตัวของตัวเอง คุณอาจรู้สึกสับสน กังวล หรือแม้แต่รู้สึกไร้หนทาง คุณไม่ได้อยู่คนเดียวในเรื่องนี้ เพราะ คู่รักและครอบครัว จำนวนมาก ต้อง เผชิญ กับความซับซ้อนของ ภาวะซึมเศร้ารอบการคลอด ซึ่งเป็นภาวะที่ส่งผลกระทบต่อคุณแม่มือใหม่หลายคน ทั้ง ในช่วงตั้งครรภ์และหลังคลอด วิธีที่ดีที่สุดในการสนับสนุนคู่ของคุณที่มีภาวะซึมเศร้ารอบการคลอดคืออะไร? คู่มือนี้มีไว้เพื่อให้คำแนะนำที่เป็นประโยชน์และเปี่ยมด้วยความเห็นอกเห็นใจ เพื่อช่วยให้คุณเป็นผู้สนับสนุนที่แข็งแกร่งที่สุดของเธอ โดยเริ่มต้นจากการทำความเข้าใจสัญญาณและก้าวแรกที่อ่อนโยนไปสู่ความชัดเจนด้วย การคัดกรองที่เป็นความลับ

การตระหนักถึงสัญญาณ: คู่ของคุณกำลังเผชิญกับภาวะซึมเศร้ารอบการคลอดอยู่หรือไม่?
เพื่อให้การสนับสนุนที่มีประสิทธิภาพ ขั้นแรก คุณต้องตระหนักว่าเกิดอะไรขึ้น ภาวะซึมเศร้ารอบการคลอด เป็นมากกว่าแค่ความรู้สึกหดหู่เล็กน้อย แต่เป็นการเปลี่ยนแปลงอย่างต่อเนื่องและมีนัยสำคัญในอารมณ์และพฤติกรรม การแยกแยะความแตกต่างจาก "อาการเบบี้บลูส์" ที่พบบ่อยกว่านั้นเป็นสิ่งสำคัญในการรู้ว่าเมื่อใดควรขอความช่วยเหลือ
นอกเหนือจากอาการเบบี้บลูส์ (Baby Blues): การแยกแยะอาการ
คุณแม่มือใหม่หลายคนประสบกับ อาการเบบี้บลูส์ (Baby Blues) ภายในสองสัปดาห์แรกหลังคลอด ซึ่งอาจรวมถึงอารมณ์แปรปรวน ร้องไห้บ่อย วิตกกังวล และนอนหลับยาก ความรู้สึกเหล่านี้โดยทั่วไปไม่รุนแรงและหายไปเองโดยไม่ต้องรักษา
อย่างไรก็ตาม ภาวะซึมเศร้ารอบการคลอด มีความรุนแรงกว่าและคงอยู่นานกว่า สามารถเริ่มต้นได้ทุกเมื่อระหว่างตั้งครรภ์หรือภายในหนึ่งปีหลังคลอด ความแตกต่างที่สำคัญคือความรุนแรงและระยะเวลาของอาการ ในขณะที่อาการเบบี้บลูส์จะจางหายไป อาการของ ภาวะซึมเศร้ารอบการคลอด (PPD) จะคงอยู่และอาจรบกวนความสามารถในการดูแลลูกและจัดการงานประจำวันของเธอ เป็นภาวะทางการแพทย์ที่แท้จริงซึ่งต้องการการสนับสนุน และบ่อยครั้งต้องได้รับการช่วยเหลือจากผู้เชี่ยวชาญ
การเปลี่ยนแปลงเล็กๆ น้อยๆ: สิ่งที่ควรสังเกตในพฤติกรรมประจำวัน
สัญญาณของ ภาวะซึมเศร้ารอบการคลอด ไม่ชัดเจนเสมอไป นอกเหนือจากความเศร้าที่คงอยู่ ให้มองหาการเปลี่ยนแปลงพฤติกรรมที่ละเอียดอ่อนเหล่านี้:
-
การเปลี่ยนแปลงการนอนหลับและความอยากอาหาร: เธอนอนมากเกินไปหรือนอนไม่หลับ แม้ในขณะที่ลูกหลับอยู่หรือไม่? ความอยากอาหารของเธอเพิ่มขึ้นหรือลดลงอย่างมีนัยสำคัญหรือไม่?
-
การสูญเสียความสนใจ: เธออาจแสดงความสนใจเพียงเล็กน้อยในกิจกรรมที่เธอเคยชอบ รวมถึงการใช้เวลากับเพื่อน งานอดิเรก หรือแม้แต่ลูกน้อย
-
ความหงุดหงิดและโกรธรุนแรง: ความโกรธหรือความหงุดหงิดที่ไม่ปกติกับเรื่องเล็กๆ น้อยๆ อาจเป็นสัญญาณอันตรายที่สำคัญ
-
ความวิตกกังวลอย่างรุนแรงหรืออาการแพนิค: สิ่งนี้สามารถแสดงออกเป็นการกังวลอย่างต่อเนื่อง ความรู้สึกว่าจะมีเรื่องร้ายแรงเกิดขึ้น หรืออาการทางกายภาพ เช่น หัวใจเต้นเร็วและหายใจถี่
-
ความรู้สึกไร้ค่าหรือรู้สึกผิด: เธออาจแสดงความรู้สึกว่าเป็นแม่ที่ไม่ดี หรือรู้สึกผิดอย่างท่วมท้นเกี่ยวกับอารมณ์ของเธอ
-
สมาธิสั้น: คุณอาจสังเกตเห็นว่าเธอมีปัญหาในการตัดสินใจหรือมีสมาธิกับงานง่ายๆ
-
การปลีกตัวจากสังคม: เธอกำลังหลีกเลี่ยงเพื่อนและครอบครัว หรือหาข้ออ้างที่จะอยู่บ้านหรือไม่?

การสังเกตเห็นสัญญาณเหล่านี้คือขั้นตอนแรกของคุณ ต่อไป ให้เริ่มต้นการสนทนาที่ให้การสนับสนุนอย่างอ่อนโยน
การสื่อสารอย่างมีประสิทธิภาพ: วิธีพูดคุยเกี่ยวกับสุขภาพจิต
การพูดคุยเกี่ยวกับสุขภาพจิตอาจรู้สึกน่ากลัว แต่การสนับสนุนที่ไม่ตัดสินของคุณสามารถสร้างความแตกต่างอย่างมากได้ เป้าหมายคือการสร้างพื้นที่ปลอดภัยที่เธอรู้สึกว่าได้รับการรับฟังและเข้าใจ ไม่ใช่ถูกวิพากษ์วิจารณ์หรือกดดัน
การเลือกเวลาและสถานที่ที่เหมาะสมสำหรับการพูดคุยอย่างเปิดอก
จังหวะเวลาเป็นสิ่งสำคัญที่สุด อย่าเพิ่งพูดถึงความกังวลของคุณในกลางช่วงเวลาที่ตึงเครียด เช่น เมื่อลูกกำลังร้องไห้หรือบ้านกำลังยุ่งเหยิง รอช่วงเวลาที่เงียบสงบและผ่อนคลายเมื่อคุณทั้งคู่พร้อมและสามารถพูดคุยกันโดยไม่มีการขัดจังหวะ เข้าหาการสนทนาด้วยความระมัดระวัง โดยเริ่มต้นด้วยประโยคที่ขึ้นต้นด้วย "ฉัน" เพื่อแสดงความรู้สึกของคุณเอง ตัวอย่างเช่น "ฉันสังเกตว่าช่วงนี้คุณดูเหนื่อยและท่วมท้นมาก และฉันก็เป็นห่วงคุณ" สิ่งนี้จะไม่เหมือนการกล่าวหา แต่เหมือนการแสดงความรักมากกว่า
การฟังด้วยความเห็นอกเห็นใจ: สิ่งที่ควรพูดและสิ่งที่ควรหลีกเลี่ยง
เมื่อเธอเปิดใจ บทบาทของคุณคือการรับฟัง ยอมรับความรู้สึกของเธอโดยไม่ต้องพยายาม "แก้ไข" ทุกอย่างทันที
สิ่งที่ควรพูด:
- "ฉันอยู่ตรงนี้เพื่อคุณ ไม่ว่าอะไรจะเกิดขึ้น"
- "ฟังดูยากลำบากมากจริงๆ ขอบคุณที่เล่าให้ฉันฟังนะ"
- "คุณไม่ได้อยู่คนเดียวในเรื่องนี้ เราจะผ่านมันไปด้วยกัน"
- "คุณเป็นแม่ที่ยอดเยี่ยม และไม่เป็นไรหรอกถ้าจะรู้สึกไม่โอเค"
สิ่งที่ควรหลีกเลี่ยง:
- "คุณควรจะมีความสุขนะ คุณมีลูกที่น่ารัก"
- "แค่ลองคิดบวกให้มากขึ้นสิ"
- "คุณแม่มือใหม่ทุกคนก็รู้สึกแบบนี้แหละ"
- "น่าจะเป็นแค่เรื่องฮอร์โมนน่ะ"
วลีเหล่านี้ แม้จะมีเจตนาดี แต่ก็สามารถลดทอนประสบการณ์ของเธอและทำให้เธอรู้สึกโดดเดี่ยวมากยิ่งขึ้นได้ ความเห็นอกเห็นใจที่เรียบง่ายและการรับฟังคือเครื่องมือที่ทรงพลังที่สุดของคุณ
การสนับสนุนที่ปฏิบัติได้จริง: วิธีช่วยเหลือในบ้าน
คำพูดสนับสนุนของคุณมีความสำคัญอย่างยิ่ง แต่ความช่วยเหลือที่เป็นประโยชน์ยังสามารถบรรเทาความกดดันในแต่ละวันที่ทำให้อาการ ภาวะซึมเศร้ารอบการคลอด แย่ลงได้ การลงมือทำแสดงให้เห็นว่าคุณคือคู่ชีวิตที่แท้จริงในการเดินทางครั้งนี้
การแบ่งเบาภาระ: เคล็ดลับการจัดการงานบ้านและดูแลลูกน้อยที่นำไปใช้ได้จริง
คุณแม่มือใหม่มักจะกำลังฟื้นตัวทางร่างกายในขณะที่ต้องรับมือกับความต้องการของทารกแรกเกิด คุณสามารถช่วยบรรเทาความกังวลได้อย่างมหาศาลโดยการรับผิดชอบงานบ้านและการดูแลลูกน้อยมากขึ้น
-
รับหน้าที่ดูแลช่วงกลางคืน: เสนอตัวรับผิดชอบการป้อนนมตอนกลางคืนหนึ่งครั้งหรือมากกว่า เพื่อให้เธอได้นอนหลับที่ยาวนานและต่อเนื่อง
-
จัดการงานบ้าน: รับผิดชอบการทำอาหาร ทำความสะอาด และซักผ้าโดยไม่ต้องรอให้เธอร้องขอ สิ่งนี้ช่วยลดภาระทางจิตใจและร่างกายได้อย่างมาก
-
เป็นผู้จัดการแขก: จัดการแขกผู้มาเยือนและการโทรศัพท์ แจ้งผู้ที่หวังดีอย่างสุภาพเมื่อเธอต้องการพักผ่อนและช่วงเวลาที่เงียบสงบ
-
ดูแลลูกน้อย: พาลูกไปเดินเล่นเพื่อให้เธอได้พักผ่อน รับผิดชอบการเปลี่ยนผ้าอ้อม อาบน้ำ และเล่นกับลูก สิ่งนี้ไม่เพียงแต่ช่วยเธอเท่านั้น แต่ยังเสริมสร้างความผูกพันของคุณกับลูกอีกด้วย

การส่งเสริมการดูแลตนเอง: ก้าวเล็กๆ ที่มีความหมาย
การดูแลตนเองไม่ใช่สิ่งฟุ่มเฟือย แต่เป็นสิ่งจำเป็นสำหรับการฟื้นตัวทั้งทางร่างกายและจิตใจ ส่งเสริมและอำนวยความสะดวกในโอกาสที่เธอจะได้ดูแลตัวเอง
- จัดสรรเวลา "ส่วนตัว" ให้เธอ: ตรวจสอบให้แน่ใจว่าเธอมีเวลาในแต่ละวัน แม้เพียง 20-30 นาที เพื่อทำอะไรบางอย่างเพื่อตัวเอง สิ่งนี้อาจเป็นการอาบน้ำอุ่น อ่านหนังสือ หรือแค่นั่งเงียบๆ
- ส่งเสริมการพักผ่อน: กระตุ้นให้งีบหลับเมื่อทำได้ จิตใจที่ได้พักผ่อนอย่างเพียงพอจะพร้อมรับมือกับความท้าทายทางอารมณ์ได้ดีกว่า
- อาหารเพื่อสุขภาพ: เตรียมหรือจัดหาอาหารและของว่างที่มีคุณค่าทางโภชนาการ เนื่องจากโภชนาการที่ดีมีบทบาทในการควบคุมอารมณ์
- การออกกำลังกายเบาๆ: ชวนเดินเล่นสั้นๆ ด้วยกัน อากาศบริสุทธิ์และการออกกำลังกายเบาๆ สามารถส่งผลดีต่อสภาพจิตใจของเธอได้
ก้าวต่อไป: การส่งเสริมให้ขอความช่วยเหลือจากผู้เชี่ยวชาญและ EPDS
แม้ว่าการสนับสนุนของคุณจะมีคุณค่าประเมินไม่ได้ แต่การได้รับความช่วยเหลือจากผู้เชี่ยวชาญมักเป็นสิ่งจำเป็นต่อการฟื้นตัว ขั้นตอนต่อไปคือการนำทางเธอไปสู่แหล่งข้อมูลที่สามารถให้ความชัดเจนและเส้นทางข้างหน้า โดยเริ่มต้นด้วยการคัดกรองง่ายๆ
เมื่อใดที่ควรแนะนำให้ขอความช่วยเหลือจากผู้เชี่ยวชาญ: การตระหนักถึงสัญญาณเตือน
หากอาการของเธอรุนแรง คงอยู่นานกว่าสองสัปดาห์ หรือหากเธอมีปัญหาในการดูแลตัวเองหรือลูกน้อย ถึงเวลาแล้วที่จะกระตุ้นให้เธอขอความช่วยเหลือจากผู้เชี่ยวชาญ สัญญาณเตือนที่สำคัญคือการพูดถึงการทำร้ายตัวเองหรือทำร้ายลูกน้อย หากเกิดกรณีนี้ขึ้น ให้ขอความช่วยเหลือทันทีจากผู้ให้บริการด้านสุขภาพหรือบริการฉุกเฉิน ยืนยันกับเธอว่าการขอความช่วยเหลือคือสัญญาณของความเข้มแข็ง ไม่ใช่ความอ่อนแอ
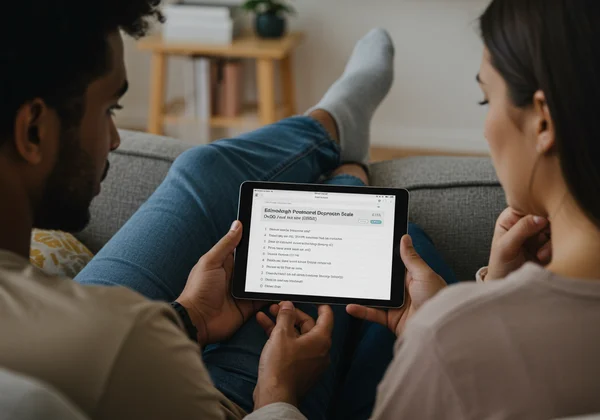
การแนะนำ EPDS: เส้นทางที่อ่อนโยนสู่ความเข้าใจ
การแนะนำให้ไปพบแพทย์อาจรู้สึกน่ากลัว ก้าวแรกที่อ่อนโยนและไม่คุกคามคือการใช้เครื่องมือคัดกรองที่ได้รับการยอมรับ แบบประเมินภาวะซึมเศร้าหลังคลอดเอดินบะระ (EPDS) เป็นแบบสำรวจง่ายๆ 10 คำถามที่ใช้โดยผู้เชี่ยวชาญด้านสุขภาพทั่วโลกเพื่อระบุคุณแม่ที่อาจมีความเสี่ยงต่อ ภาวะซึมเศร้ารอบการคลอด
คุณสามารถแนะนำอย่างอ่อนโยนว่า "ฉันเจอเครื่องมือออนไลน์ที่เป็นความลับนี้ที่ช่วยให้คุณแม่มือใหม่เข้าใจความรู้สึกของตัวเองได้ มันฟรีและเป็นส่วนตัวมากๆ บางทีเราลองมาดูกันหน่อยไหม?" สิ่งนี้จะวางตำแหน่ง แบบทดสอบ EPDS ออนไลน์ฟรี ไม่ใช่เป็นการวินิจฉัย แต่เป็นวิธีรวบรวมข้อมูล การทำแบบคัดกรอง EPDS ออนไลน์นั้นรวดเร็ว (3-5 นาที) ไม่ต้องลงทะเบียน และให้คะแนนและการตีความผลทันทีเมื่อเสร็จสิ้น คะแนนนี้สามารถเป็นจุดเริ่มต้นที่มีคุณค่าสำหรับการสนทนากับแพทย์หรือนักบำบัดได้
คุณไม่ได้อยู่คนเดียว: บทบาทของคุณในการเดินทางสู่สุขภาพที่ดีของเธอ
การสนับสนุนคู่ของคุณที่กำลังเผชิญกับ ภาวะซึมเศร้ารอบการคลอด เป็นการวิ่งมาราธอน ไม่ใช่การวิ่งระยะสั้น ความอดทน ความเห็นอกเห็นใจ และความช่วยเหลือที่เป็นประโยชน์ของคุณเป็นสิ่งจำเป็นต่อการฟื้นตัวของเธอ อย่าลืมดูแลสุขภาพจิตของตัวคุณเองด้วย – หากตนเองไม่พร้อม ก็ไม่สามารถช่วยเหลือผู้อื่นได้ คุณเป็นส่วนสำคัญของกระบวนการเยียวยา ด้วยการตระหนักถึงสัญญาณ การสื่อสารด้วยความเห็นอกเห็นใจ และการส่งเสริมให้ก้าวแรกอย่างกล้าหาญ คุณสามารถช่วยนำทางเธอกลับสู่สุขภาพที่ดีได้
กระตุ้นให้เธอ ก้าวแรก ในวันนี้ มันเป็นการกระทำที่เรียบง่ายแต่ทรงพลังที่สามารถเปิดประตูสู่การสนับสนุนและการเยียวยาสำหรับทั้งครอบครัวของคุณ
คำถามที่พบบ่อยเกี่ยวกับการสนับสนุน ภาวะซึมเศร้ารอบการคลอด
ฉันควรทำอย่างไรหลังจากคู่ของฉันได้คะแนน EPDS สูง?
คะแนน EPDS ที่สูงบ่งชี้ถึงความเสี่ยงอย่างมีนัยสำคัญของภาวะซึมเศร้า และหมายความว่าถึงเวลาปรึกษาผู้เชี่ยวชาญด้านสุขภาพ ใช้คะแนนดังกล่าวเป็นจุดเริ่มต้นของการสนทนากับแพทย์ สูตินรีแพทย์ หรือนักบำบัดสุขภาพจิต รายงานจากการคัดกรอง EPDS ของคุณสามารถให้ประเด็นในการพูดคุยได้ โปรดจำไว้ว่าเครื่องมือนี้ใช้สำหรับการคัดกรอง และผู้เชี่ยวชาญสามารถให้การวินิจฉัยที่แม่นยำและแผนการรักษาได้
แบบทดสอบ EPDS สามารถคัดกรองความวิตกกังวลได้ด้วยหรือไม่?
แม้ว่า EPDS จะออกแบบมาเพื่อคัดกรองภาวะซึมเศร้าเป็นหลัก แต่คำถามบางข้อ (เช่น เรื่องความวิตกกังวลและอาการแพนิค) ก็สามารถช่วยระบุอาการของความวิตกกังวลหลังคลอดได้ ซึ่งมักเกิดขึ้นพร้อมกับภาวะซึมเศร้า ผู้เชี่ยวชาญสามารถให้การประเมินที่ครอบคลุมสำหรับทั้งสองภาวะหลังจากที่คุณใช้ เครื่องมือคัดกรองของเรา
แบบทดสอบ EPDS ใช้เวลาทำนานแค่ไหน?
การคัดกรอง EPDS ออกแบบมาให้รวดเร็วและเข้าถึงได้ง่ายสำหรับคุณแม่มือใหม่ที่มีเวลาจำกัด แบบทดสอบ 10 คำถามบนแพลตฟอร์มของเราโดยทั่วไปใช้เวลาเพียง 3 ถึง 5 นาทีในการทำ โดยให้คะแนนและการตีความผลทันทีเมื่อเสร็จสิ้น
เครื่องมือคัดกรอง EPDS ออนไลน์นี้ฟรีจริงหรือไม่?
ใช่ ฟรีอย่างแน่นอน เครื่องมือคัดกรอง EPDS ฟรีที่มีอยู่บนเว็บไซต์ของเรานั้นฟรีอย่างสมบูรณ์ เป็นความลับ และไม่ต้องลงทะเบียนใดๆ เป้าหมายของเราคือการทำให้ก้าวแรกที่สำคัญในการระบุความเสี่ยงของ ภาวะซึมเศร้ารอบการคลอด เข้าถึงได้ง่ายที่สุดสำหรับทุกคน ทุกที่